The 14-20th March 2022 was Healthcare Science Week – a week dedicated to raising awareness of the amazing work of healthcare science professionals, and celebrating the impact they have on patient care. Did you know that there are over 50,000 healthcare scientists working in the NHS and public health services in 50 different specialisms? The work of healthcare scientists underpins 80% of all diagnoses. For each day of HCS Week 2022, we posted a ‘Day in the Life’ of a different healthcare scientist on our Twitter and Instagram channels. See the whole week collated here!
With thanks to Ruth Braham, Katie Cheswick, Rachael Franklin, Charlotte Jones, Gabriel Santos, Alex Shaw and Linda Shi.
MONDAY: Vascular Science
Vascular science is about the assessment of how blood flows in the body through arteries and veins which can be scanned and visualised in real-time using an ultrasound machine.
An ultrasound scan requires hand-eye coordination and dexterity for moving the ultrasound probe over a patients’ skin to detect their blood vessels which can be viewed on a digital screen. During these scans, vascular scientists use their knowledge of haemodynamic, ultrasound physics and vascular disease to assess blood vessels for plaque build-up, blood clots, aneurysms and measure parameters of blood flow. Such scans assist with the diagnosis of vascular disorders, including transient ischaemic attack (TIA), stroke, aneurysm, peripheral disease, deep vein thrombosis and varicose veins.
Our day-to-day role involves interacting with patients, particularly the elderly and those with disabilities and pre-existing health conditions. Responsibilities include taking patient history, performing ultrasound scans and reporting results to referring clinicians such as vascular surgeon’s, radiologist, specialist nurses or GPS.
TUESDAY: Clinical Engineering

As a Clinical Engineering STP trainee you could be working in a variety of roles. In a hospital, the Clinical Engineering team will typically be involved in managing the operations and logistics of all the medical devices used within the hospital. But Clinical Engineers can also be found in Rehabilitation Engineering services where they work to provide customised wheelchair seating, orthotics and communication aids to patients. Additionally, Clinical Engineers work in patient facing roles across a wide range of Clinical Measurements services, such as Gait Analysis, Urodynamics, GI and much more. Here Clinical Engineers apply their understanding of Physics and Engineering principles, alongside their anatomical knowledge, for diagnosis, monitoring and treatment of patients.
As a Clinical Engineering STP trainee specialised in Clinical Measurement, I spend the majority of my time in a paediatric gait laboratory. Roughly 40% of my time is spent in patient appointments, 40% on processing and reporting on the data gathered and the remaining 20% of time is spent on research projects or MSc commitments. Gait analysis appointments last between one and half to two and half hours and involve a variety of different measurements; motion capture technology is used to perfectly record the way an individual walks in 3D space, then additional measures of the electrical activation of the muscles and forces generated during walking are taken alongside the passive range of muscles and ultrasound imaging of the muscles. These measurements are all used to explain why a patient walks in a particular way and how they can walk more easily and comfortably.
WEDNESDAY: Ophthalmic and Vision Science
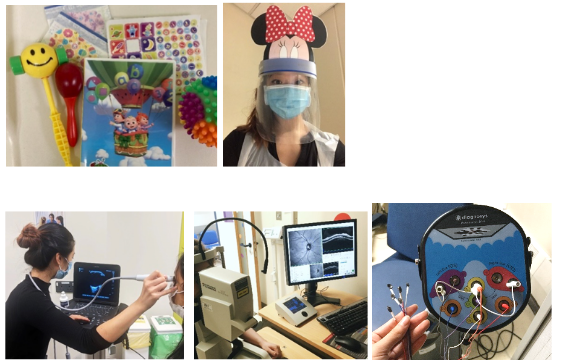
Hi I’m Linda and I’m a 3rd Year NHS STP trainee in Ophthalmic & Vision Science (OVS) at Great Ormond Street Hospital for Children NHS Foundation Trust. As OVS scientists, we carry out lots of different specialised tests to investigate the eyes and visual pathway (from retina to brain) – to help diagnose different conditions that might affect how someone sees!
We start the day by powering up our necessary equipment and performing daily checks. This is important to make sure all components are working, electrically safe, and properly calibrated to ensure accuracy of our results. We look through our patients booked for the day to get an understanding of their medical history, reason for referral, and any special adjustments they might need. We see children of all ages (from tiny babies to teenagers), and of all levels of vision, abilities and backgrounds – so we need to tailor our investigations both to the individual patient and to the diagnostic question.
As you can imagine, getting an active toddler to cooperate with tests that require lots of staying still is not always easy! We work together closely and dynamically as team with colleagues and parent/carers to help obtain the best data we can, as well as make the appointments fun for the young patient. Luckily, we’re well-stocked with toys, stickers, cartoons and songs.
The appointment might involve visual electrophysiology tests, ultrasound imaging, colour vision testing, eye-movement recordings, and/or retinal imaging. We then analyse and interpret the data to produce a clinical report of our findings, which the referring clinician will use to guide discussion during the consultation with the patient and their family.
As an STP trainee, as well as my daily clinical role, I have training and competencies to complete towards my portfolio, and sometimes academic teaching as part of the MSc, as well as my own research project. There are also additional opportunities to be involved in clinical research, audits and innovation, and healthcare science outreach. It’s a varied, exciting role where you’re learning every day, and using your knowledge and skills to benefit patient management.
THURSDAY: Genomics

First of all – what is genomics?
Genomics is the term used to refer to the study of the human genome. Whilst this field can also be referred to as genetics, genomics is now more widely used to reflect changes that have occurred in the field as we have moved from looking at individual genes to looking at large panels of different genes. Whilst this has greatly improved our ability to diagnose patients it has also provided new challenges.
Currently I’m on placement in the inherited cancer team, this largely involves analysing panels of genes associated with inherited high-risk of cancer, looking at the results of panels and classifying variants according to standardised criteria, looking at things like the prevalence in healthy individuals and those with cancer, functional analyses and information published about the variant. All this helps us to decide whether the variant is or isn’t disease causing. Complex cases are discussed at a regular Multidisciplinary team meetings to ensure a wide variety of expert input. Once any variants have been classified, I write the patient’s reports stating what has been found and what this means for them and their family
Throughout the STP I have worked in a wide variety of different teams looking at a wide range of different conditions and at test methodologies. From looking at the whole genome for large scale changes using Microarray or Karyotyping to single gene sequencing for specific conditions.
When performing any test it is important to understand what results mean for the patient and the benefits and limitations of the specific test used, all this information should be included on the patients report. It is also important to understand the technological aspects of testing and what quality control methods there are in place to make sure testing is accurate.
Whilst we don’t usually come into direct contact with patients the patient is always at the heart of the diagnostic service. In the first year of my training, I spent time with the Genomic Counselling service, who help patients and families through the testing process. This highlighted the importance of these results and the genuine impact these have on patients’ lives, and the impact on the patient’s sense of identity, their relationships, and their experience with genetic disease.
Overall, I am thrilled to be part of such an important and rapidly changing service and am looking forward to seeing what new opportunities and challenges the coming years bring.
FRIDAY: Medical physics

Hi, I’m Rachael and this is a day in the life of an Imaging with Non-Ionising Radiation STP Trainee. My Medical Physics specialism covers MRI and Ultrasound Imaging, so my teams provide Physics and other technical support to radiographer, sonographer, radiologists, and other users of these scanners.
My days involve setting up new MRI pulse sequences, to improve the clinical imaging or for research studies; QA and acceptance testing, using test objects to measure the performance of scanners; providing safety advice, training, developing safety policies and performing audits, to ensure patients and staff are receiving and performing these scans safely;
troubleshooting scanner problems; planning service improvements and undertaking research projects, such as establishing new QA procedures, to evaluate and expand our clinical services; and post-processing clinical scans.
SATURDAY: Cardiac Physiology
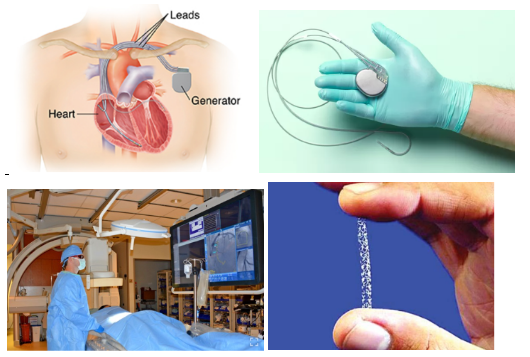
Cardiac physiologists are involved in the diagnosis and treatment of patients with heart conditions. I have chosen to specialise in cardiac rhythm management rather than echocardiography (ultrasounds of the heart). In cardiac rhythm management I perform and support a wide range of non-invasive and invasive procedures. My time is mainly split between pacing clinic and the catheterisation labs. In pacing clinic, we review patients with pacemakers and implantable defibrillators. We perform a range of tests to ensure the battery and leads that go into the heart are working well. Additionally, we assess patients’ symptoms and any stored arrhythmias. Based on all of these we may make changes to the device settings and programming if required.
In the catheterisation labs patients undergo a large variety of minimally invasive procedures that uses x-rays to guide the procedure. Small tubes (called catheters) are inserted via veins or arteries and fed into the heart. A common procedure is unblocking coronary arteries using small balloons and stents to hold the artery open, helping to prevent or treat a heart attack. Other procedures include pacemaker insertion or battery change, valve replacements, measuring the pressures in the heart and ablations (burning or freezing small sections of the heart to help stop irregular heart rhythms). While the consultant performs the procedure the role of the cardiac physiologist is to monitor the patients haemodynamic and ECG, perform additional tests, get equipment and write the report.